
Seven years ago, Robert Kerley, who makes his living as a truck driver, was loading drywall when a gust of wind knocked him off the trailer. Kerley fell 14 feet and hurt his back.
For pain, a series of doctors prescribed him a variety of opioids: Vicodin, Percocet and Oxycontin.
In less than a year, the 45-year-old says he was hooked. “I spent most of my time high, laying on the couch, not doing nothing, sleeping, dozing off, falling asleep everywhere,” he says.
Kerley lost weight. He lost his job. His relationships with his wife and kids suffered. He remembers when he hit rock bottom. One night hanging out in a friend’s basement, he drank three beers. The alcohol reacted with an opioid he was on and soon he was fighting to breathe.
“I was taking so much morphine that I respiratory arrested because of it,” Kerley said. “I stopped breathing.”
An ambulance arrived, and EMTs administered the overdose reversal drug Naloxone. Kerley was later hospitalized. As the father of a 12-year-old son, he knew he needed to turn things around. That’s when he signed up for Kaiser Permanente's Integrated Pain Service.
“After seven years of being on narcotics and in a spiral downhill, the only thing that pulled me out of it was going to this class,” he says. “The only thing that pulled me out of it was doing and working the program that they ask you to work.”
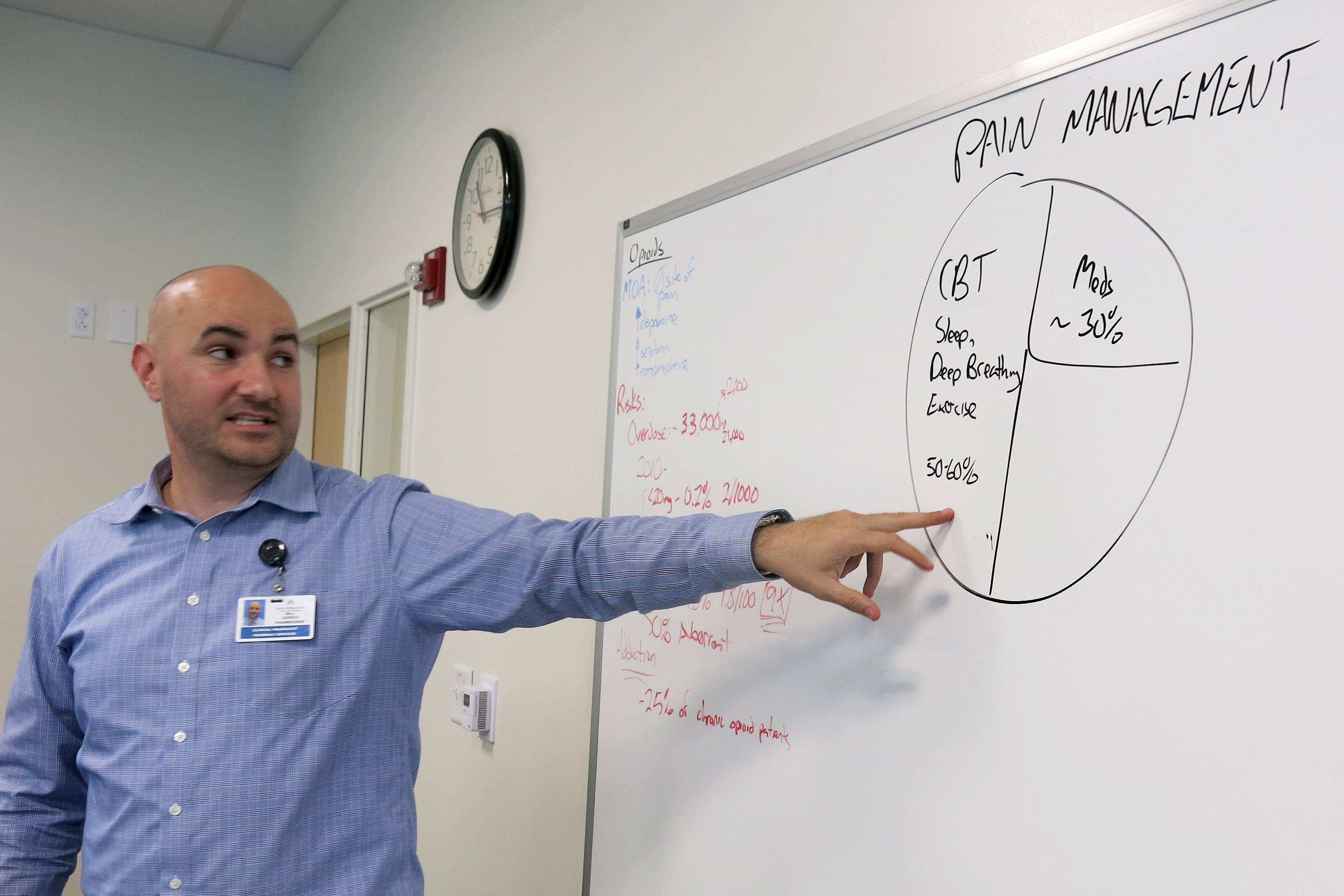
It’s an eight-week course, available to Kaiser members for $100, that’s designed to educate high-risk opioid patients about pain management. A recent class met at Kaiser’s Rock Creek medical offices in Lafayette. Will Gersch, a clinical pharmacy specialist, was teaching several students battling addiction the science behind prescription drugs.
“So basically the overarching message here is the higher the dose of the opioids, the higher the risk,” he told the group, as he jotted down numbers on a whiteboard. “If you're over these two doses, that's a risk factor.”
Upstairs, his colleague Amanda Bye, a clinical psychologist, highlighted a key element of the program: It’s integrated. Bye says on one floor, there’s a doctor, a clinical pharmacist, two mental health therapists, a physical therapist, and a nurse.
“We brought in all these specialists. We all know the up-to-date research of what's most effective in helping to manage pain,” Bye says. “And that's how the program got started.”
Kaiser tracked more than 80 patients over the course of a year. It found the group’s ER visits decreased 25 percent. Inpatient admissions and total opioid doses dropped 40 percent.

Bye says the team helps patients taper off opioids and explore the benefits of alternatives like exercise, meditation, acupuncture and mindfulness. “And we found that we've had really good results getting those patients unstuck from the mud, getting them moving and living the life they want to live,” Bye says.
Family medicine Dr. Heidi Clune says sometimes a simple pain prescription can escalate to addiction.
“Our goal with all of our treatment is to take that patient off that opioid Island and build that bridge, and get them back to functioning with society,” Clune says.
Early data shows the program has reduced costs, Clune says. Similar projects in California showed a reduction in the number of prescriptions and pills per patient, says Kelly Pfeifer, director of high-value Care at the California Health Care Foundation. Her group released case studies of three programs, like Kaiser’s Colorado program.
“We've seen great success with these models that are integrating complementary therapy, physical therapy, behavioral health, and medical care,” Peiffer says. A key strategy is to gradually decrease the amount of opioids a patient takes, rather than cut them off before they’re ready. “It works so much better when the patients have access to these complementary therapies,” she says. “And it works even better when those complementary therapies are part of an integrated team.”
One challenge is scale. Big systems like Kaiser are the ones that have ample resources and can afford programs like this. Another is payment. Some insurers won’t pay for some alternative treatments, others have separate payment streams for different kinds of care.
“Frequently behavioral health and medical health are paid for by entirely different systems,” Peiffer says.
The need for programs like Kaiser’s is urgent. In 2016, a record 912 people died from an overdose in Colorado, according to data recently released by the state health department. Three hundred people died from an opioid overdose. Opioid use often leads to an addiction to heroin, which claimed another 228 lives last year in the state. Those two causes together now rival the number of deaths from diabetes, car accidents, or chronic liver disease.
Kaiser’s Integrated Pain Service has given some patients a second chance. Robert Kerley, now a veteran of the program, recently shared his story with other patients. “I got my life back. I can sleep. I can eat. I can enjoy things,” Kerley told them.
To cope with pain, Kerley starts his morning with stretching and a version of Tai-chi that he calls “My-chi.” He practices deep breathing. His advice to others suffering from pain or addiction?
“Do whatever it takes to walk away from it, like no matter what,” Kerley said. “Trust me, it gets better. It gets 100 percent better than where you're at right now.”
Better for Kerley means his relationships with his family have improved. And he’s back at work, once again able to make a living as a truck driver.








