
How do you solve a problem like Colorado’s teen vaping rate, the highest in the nation?
That’s the question lawmakers are gathering on Wednesday to try and answer. They’ll be asking questions about all things vaping as they consider new measures to stop the epidemic, including what the science shows about health risks.
A group of doctors at Children’s Hospital Colorado had a few insights they'd like to offer.
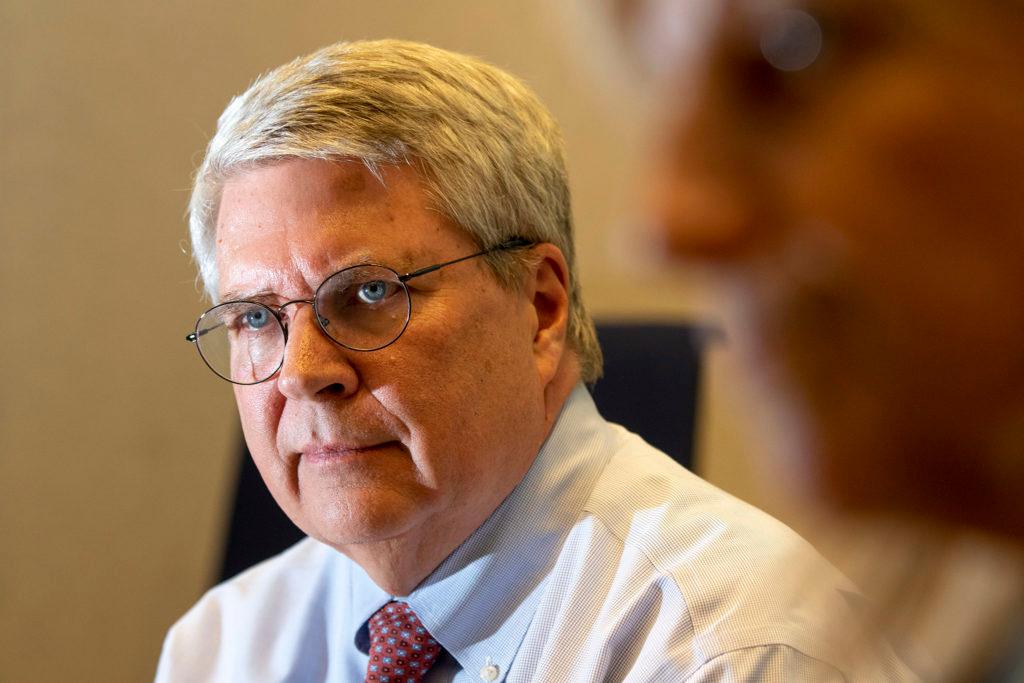
Among them was lung expert Dr. Robin Deterding who, when it comes to talking about the health risks of vaping, is blunt.
“You're inhaling a chemistry experiment,” Deterding said. “And that's bad for your lungs."
Companies marketed vape pens as a safer alternative to cigarettes, but the research that’s emerging suggests some of the potential dangers are similar. Take for example the puffy clouds that come out of a vape device, known as second-hand vapor.
“I think we do believe second-hand vape smoke can stimulate asthma exacerbations of asthma problems,” said Deterding, who is the medical director of the Breathing Institute and chief of Pediatric Pulmonary Medicine at Children’s Hospital Colorado.
Those clouds contain potentially harmful substances.

When we asked CPR’s audience what they wanted to know about the health risks of vaping, one wondered: “What are the long-term side effects of nicotine addiction once a child has started vaping?”
It’s a critical question, since “the magnitude of the number of our youth that are participating in some degree of vaping is extraordinary,” Deterding said.
Many teens believe they’re inhaling harmless water vapor. But it can actually contain high concentrations of nicotine as well as particles linked to lung disease and cancer. The doctors say vaping impacts young people in at least three key areas: the lungs, the heart and the brain.
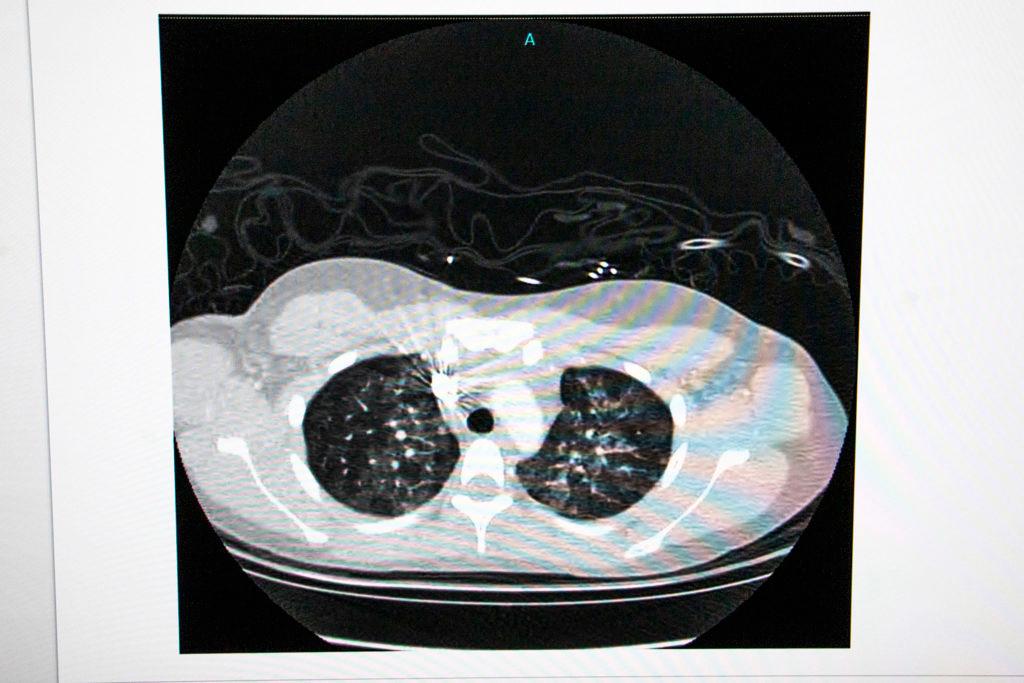
First, the lungs, where those foreign substances can harm tiny, delicate airways, Deterding said.
“If you're going to do it long term? We're seeing some of these airways you have air tubes that lead out to these air sacs and the cells in those air tubes are also being damaged,” she said.
It was this kind of damage that caused the recent rash of vaping-linked lung illness, hospitalizing more than 2700 people and leading to 64 deaths. Health officials blame vitamin E acetate, an additive in some THC-containing e-cigarettes, as the culprit in many cases. Another study has found a link between vaping and increased odds of asthma and chronic lung disease. Long-term risks are real because the lungs are so sensitive.
“Once you start a scarring process, it's very difficult to reverse,” Deterding said.
Beyond the lungs, research suggests vaping may also be bad for the heart as well.
“We know that cigarette smoking has a very negative impact on the arteries and the heart,” said Steve Daniels, the pediatrician-in-chief at Children’s Hospital Colorado and the chair of the CU Anschutz Medical Campus’ pediatrics department.
Cigarettes can raise blood pressure and heart rates and can cause vascular disease. Scientists aren’t sure if the same is true for e-cigarettes, but more and more studies are raising alarms, Daniels said. One last year found adults using e-cigarettes had higher risks of heart attack and coronary artery disease compared with non-users.
Daniels said more research is still needed.
“(Vaping) hasn't even been around long enough to know what the chronic effects might be, but maybe we don't even need to know that because we do know that for those who are vaping nicotine, it's incredibly addictive,” he said.
That gets to e-cigarettes’ third big health risk: addiction, to which teens are especially vulnerable. The e-cigarette industry says its products are meant to help adults quit smoking. But Daniels said many young vapers will go on to become smokers.
“Kids, as they become adults, may switch to smoking and then we know very well what the impacts of that are,” he said.
Nicotine can harm adolescent brain development and alter brain chemistry. Child psychiatrist Joel Stoddard said that, at least in research on young animals, “there are permanent changes in neural pathways for attention and memory.”

“And it makes you more prone to goosing that reward system,” Stoddard said.
That means teens who vape aren’t just at risk for nicotine addiction. They’re also vulnerable to mood disorders and reduction in impulse control. Nicotine can also impact attention and learning.
So, how do we help young people quit vaping, another CPR listener wondered.
It's a good question, Stoddard said. And a hard one.
“There's not a lot of good evidence for any kind of treatment,” Stoddard said.
There have been decades of investigation into quitting smoking traditional cigarettes, and Stoddard suspects some of those programs and medications may well work for young vapers.
“The goal now is to find out what parts of those work, translate them over for vaping, and to implement those programs on the treatment side. And of course, we need the prevention in the first place,” he said.
Another CPR listener wanted to know which is really worse: vaping or cigarettes. Daniels says though more is known about cigarettes, “the answer is they're both bad."
"And they may be extra bad because they reinforce each other, and you almost can't think of one without the other," he said.
If you look at all the bodily systems affected, neither has a place in a healthy lifestyle, Daniels said.
With cigarettes, peer pressure and support can help teens quit, Stoddard said. But with vaping, that’s a challenge, since so many young people are doing it.
Another obstacle is the scale of the problem, Daniels said.
“When you think about 10 percent of middle schoolers and 30 percent of high schoolers (who regularly use e-cigarettes), that's a fair number of kids that need help now,” he said. “I think it's a public health emergency.”
Stoddard agreed, noting one key study that found the rate of teens vaping nicotine had shot up in an unprecedented fashion.
“In the 45 years the survey has been going on, no other substance has risen so high in so short a time,” Stoddard said.









