Scott Kaplan was diagnosed with COVID-19 on March 26.
He deteriorated quickly. Just a day after his diagnosis, he was hospitalized, sedated and placed on a ventilator. His kidneys started to fail, so he was put on dialysis. He was put on an ECMO machine, an advanced type of mechanical life support that removes blood from the body, oxygenates it and then returns it, allowing Kaplan’s lungs to recover.
His family took to social media and local news to share their story and seek convalescent plasma, a treatment that’s shown promise in treating COVID-19 patients. A donor was found.
On April 5, he was given convalescent plasma from a donor who recently recovered from the novel coronavirus.
At first, the changes were small and hard to detect. On Monday, doctors lowered the paralytic he was on. Kaplan got a phone call from his family, said his sister, Marci Kaplan.
“He was able to respond to verbal commands. He was able to wiggle his toes, open his eyes, and then about eight or nine of us did a conference call with him,” she said. “He got to hear our voices and he was able to acknowledge that he heard us. He got to hear his children's voices.”
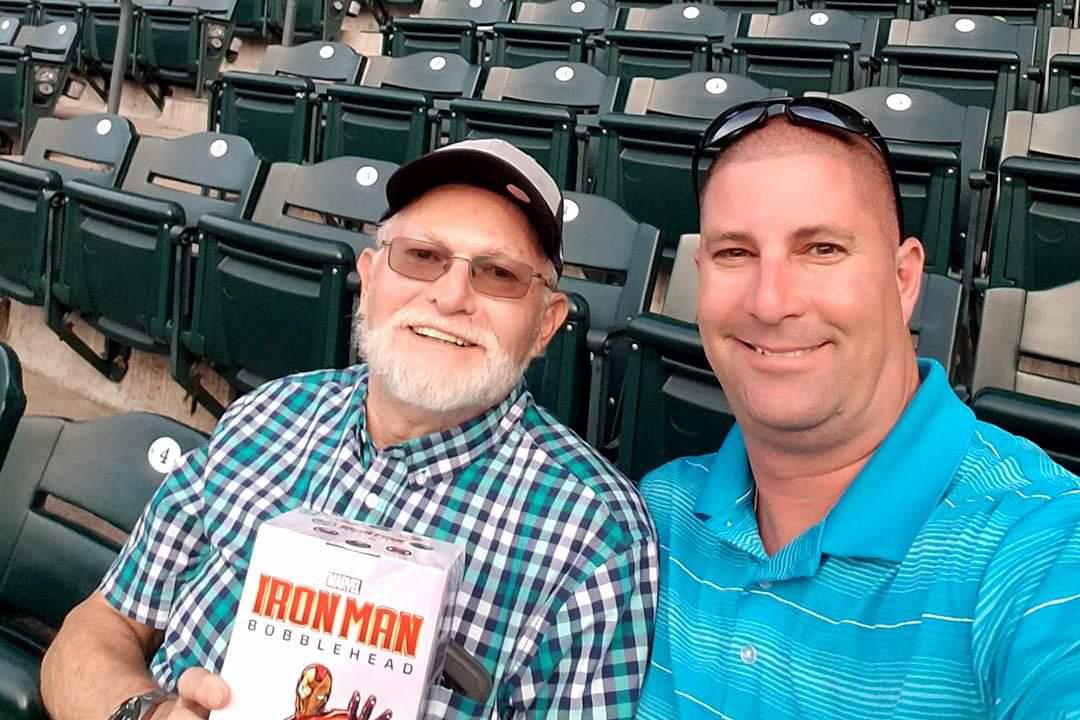
Kaplan, 43, who has two sons, 14-year-old Patrick and 11-year-old Ethan, with his wife, Denise, is not out of the woods yet.
But as COVID-19 has claimed more than 200 lives in Colorado and nearly 15,000 nationwide, the early results in Kaplan’s case are offering maybe just a little hope to researchers and doctors looking for treatments. Plasma is the yellowish-liquid part of the blood that carries cells and proteins throughout the body. It also contains antibodies from every cold, flu or allergen the donor has ever faced, and that includes antibodies to COVID-19.
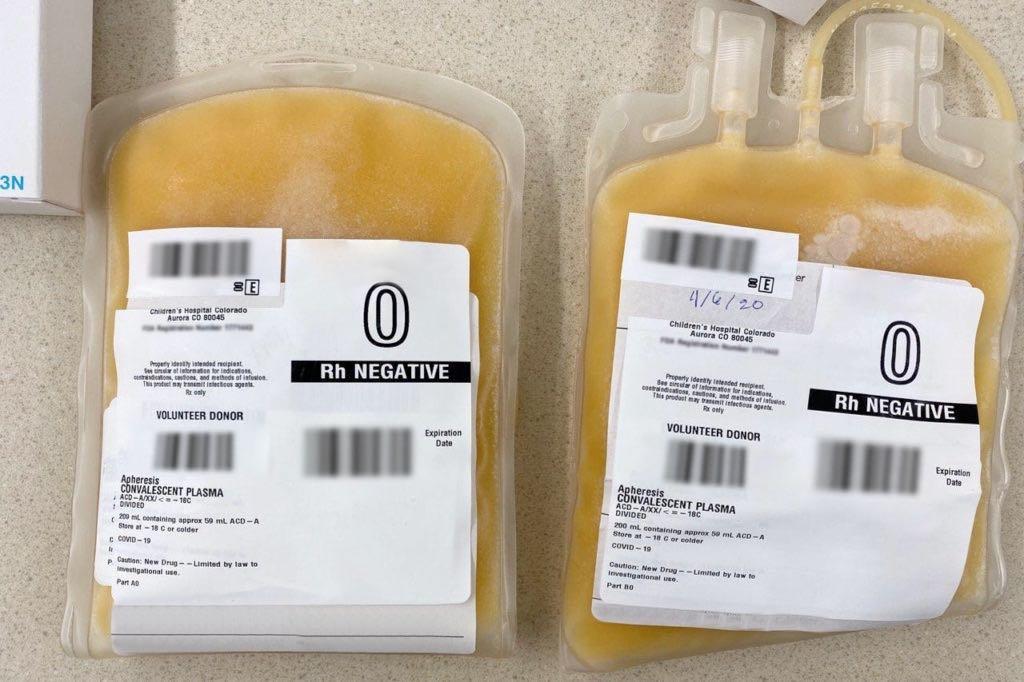
In early March, Dr. Kyle Annen, medical director of the blood collection center at Children’s Hospital of Colorado, heard about the possibility of using convalescent plasma in COVID-19 patients. She started preparing her donation center to accept donations from donors who have recovered from the virus around the same time the Food and Drug Administration released its guidelines for giving convalescent plasma to COVID-19 patients.
Then, Annen got a call from Dr. Mary Berg, medical director of transfusion services at University of Colorado Hospital. There was a patient who was a good fit for convalescent plasma.
Annen was able to secure a donor who recovered from COVID-19, test them to ensure they were negative for the virus, and then process the plasma in line with federal guidelines to get it to the patient in need, Dr. Michael Leonard, a 68-year-old anesthesiologist and businessman from Evergreen.
“I mean we really just were able to put a rush on things when we felt that they were a priority,” Annen said. “This convalescent plasma collection was an example of that. My team was all hands on deck ready to go. Everyone recognized how significant this was and how important this was for this patient.”
The results, like in Kaplan’s case, are not yet clear. Like Kaplan, Leonard was also put on a ventilator after being admitted with a persistent violent cough, fever and extreme shortness of breath. He is taking other experimental treatments in addition to the convalescent plasma, and doctors are hopeful that one of those treatments will make a difference.
“We are hoping that it's something that's going to be beneficial, but it definitely needs to be studied more. It's not something that we can just assume that is going to be the magic bullet that's going to cure everything,” said Berg. “ It was not shown to be effective in other types of viral infections, and so we're not really sure how this is going to go.”
There’s anecdotal evidence that plasma was used to treat sick people during the 1918 Spanish Flu, Berg said. It was also used successfully to treat H1N1 flu in 2009-10. But in other cases it’s not been effective.
UCHealth has given plasma to a handful of patients, and each time they’ve had to fill out an emergency investigational new device form with the FDA, which allows doctors to apply to use plasma on a case by case basis. An eIND has to be filled out for each patient, but, Berg said, UCHealth researchers are working on the application to start a plasma trial which would allow them to treat more patients and start to better understand the treatment’s efficacy.
But, Berg cautioned that ramping up these efforts won’t happen overnight.
“The idea of trying to collect this convalescent plasma on a large scale is completely new to our blood collection system.” she said. “There are a lot of bugs in the process that need to be worked out before we can really process donors and get those donors in the numbers that we would really like to and in the numbers that I think would be helpful to the most number of patients. We can't just collect people and worry about the testing later.”
To donate convalescent plasma to a COVID-19 patient, the donor needs proof of a positive COVID-19 test and then proof that they subsequently tested negative for the virus. Berg said they have to be sure the donor tested positive for coronavirus because there’s no certain antibody test, which would allow blood collection centers to test for coronavirus antibodies. Flu is still going around, so having had symptoms of coronavirus isn’t enough to prove someone has had it. Children’s and UCHealth don’t expect to have antibody tests for a few more weeks.
While Colorado hospitals and researchers work toward improving the blood collection system and getting approval from the FDA for trials, patients like Kaplan and his family are waiting to see if the treatment worked.
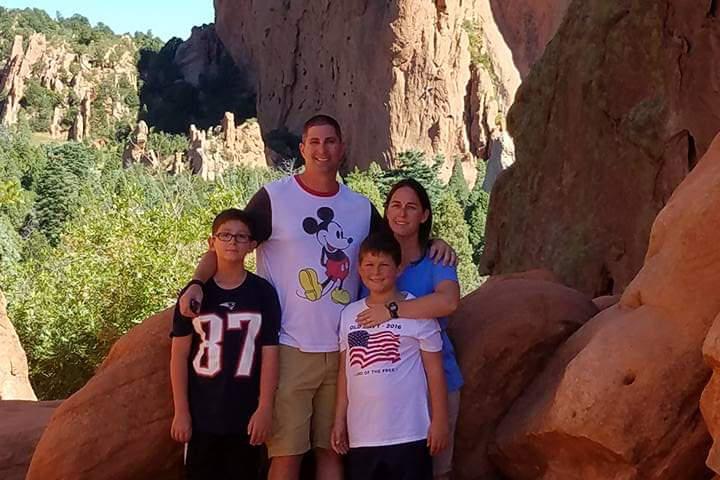
“He's just very giving, very caring. He's charismatic, he's great with his words. Everybody just has always loved him, and Marci and I have always looked up to him,” said Kaplan’s other sister, Samantha Dunham. “He's always been a great father, great husband, great friend and somebody you can always turn to.”
Seventeen years ago, Kaplan was diagnosed with Multiple Sclerosis, which put him at a higher risk for suffering severe side effects with COVID-19. Even when his MS was at its worst, he continued to coach his kids’ teams and take on whatever he put his mind to.
“For something like this to completely stop him when MS has never even stopped him, it's just, it's hard,” Dunham said.
When the coronavirus pandemic first took hold in the U.S., Dunham said she brushed it off. Then when state’s started to roll out stay at home orders, she continued to question the validity of the alarm bells.
“I didn't stop going to work. I did not stop living my life, going out in public, and hanging out with like a small group of friends. I did everything you're not supposed to,” Dunham said. “Two days prior to my brother getting sick, my husband and I looked at each other and said, 'Isn't that weird? We don't know anybody who has this.' And then two days later our brother gets sick, not just sick, but this man is fighting for his life, and there's still no confirmation that he's even gonna make it out.”
Now, both of Kaplan’s sisters worry about the people they see who aren’t wearing masks, aren’t social distancing, and who call the virus “a little cold.”
“Don't take my brother's story with a grain of salt. Take it seriously,” Marci Kaplan said. “My brother was living his everyday life, and that's how he got sick. It is not a cold. It is the worst thing that somebody could get.”









