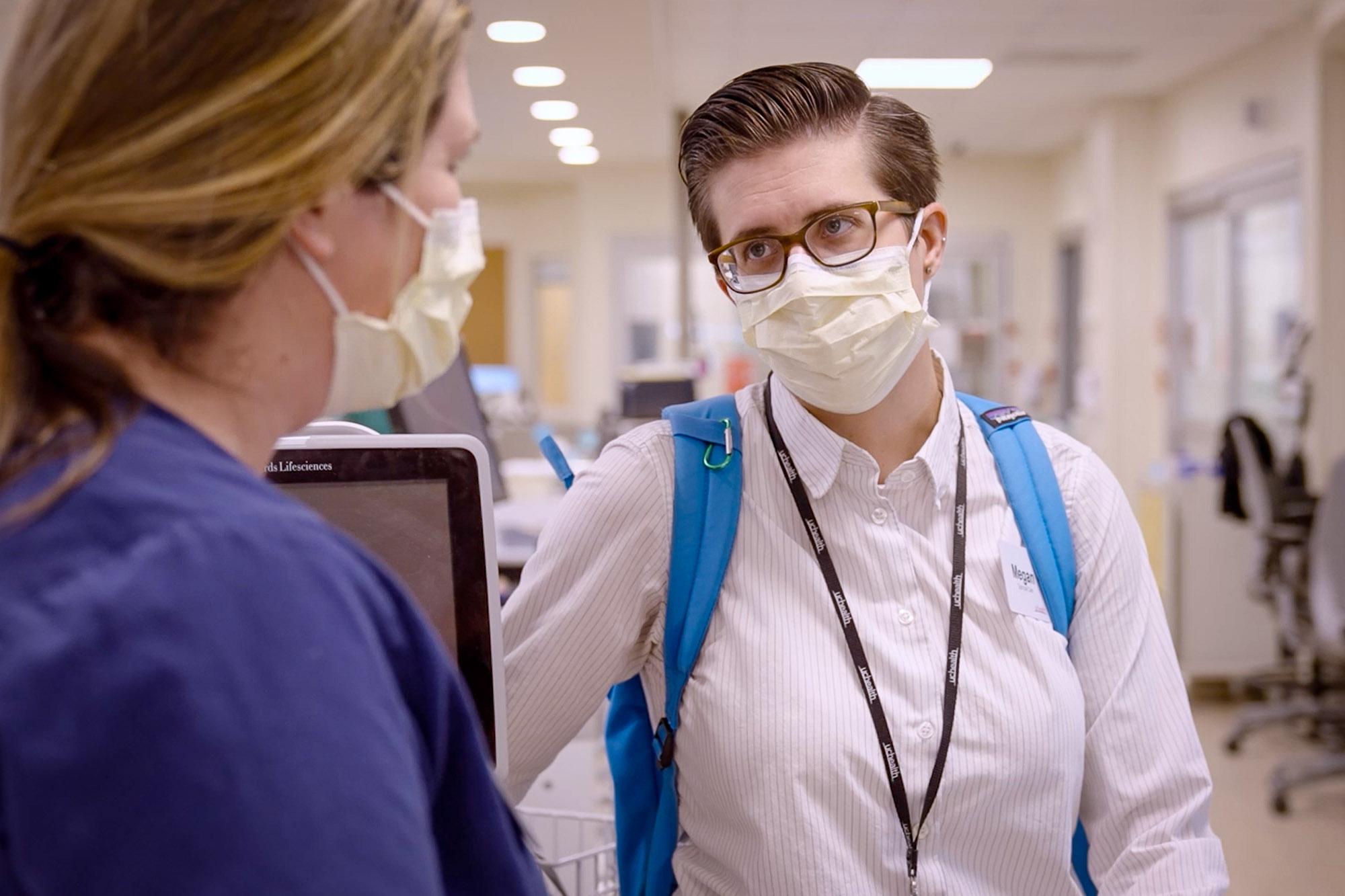
Colorado hit a grim pandemic milestone Tuesday, surpassing 10,000 deaths from the coronavirus. One person who has worked on the frontlines of that crisis is Megan Worthman. She’s a staff chaplain who works for UCHealth at the University of Colorado Anschutz Medical Campus. She spoke with CPR Health Reporter John Daley about the milestone, how she deals with families of loved ones at the hospital and how she's had to be a source of support for stressed out healthcare workers.
Daley's questions are in bold letters.
I wonder if you could just reflect on the fact that we've now reached 10,000 deaths due to COVID and Colorado.
It's really staggering to realize that, you know, I've met a lot of those people affected. I've met probably in the thousands of those people. And I know their families, I know their names. I mean, these are real people. This isn't just a number to me it's just really heart wrenching. And I don't know what the future looks like. That number will continue to climb. And I just know that means more heartbreak.
How would you describe the impact of those losses on the families that you've worked with, the patients that you've worked with and the community?
It is hard to understate the wonderful people that have been affected by this and that we've lost, but it's also the people that have survived and are living with significant debilitation. That number just doesn't even adequately reflect how many people are affected. I don't even have words to describe just how this has torn families apart. I think that that has really been lost in how the pandemic has been politicized. These are grandmas and grandpas and moms and dads and sons and daughters. It's not just one demographic affected.
I wonder if you could tell me a little bit more about what you think has been lost as the pandemic has become politicized?
I think we've lost the perspective that these are real people, that these aren't just political numbers. And, uh, you know, these are people who are not showing up their graduations or holidays anymore. These are real empty seats at the table.
Tell me how you're counseling people and how that play is out in the hospital setting?
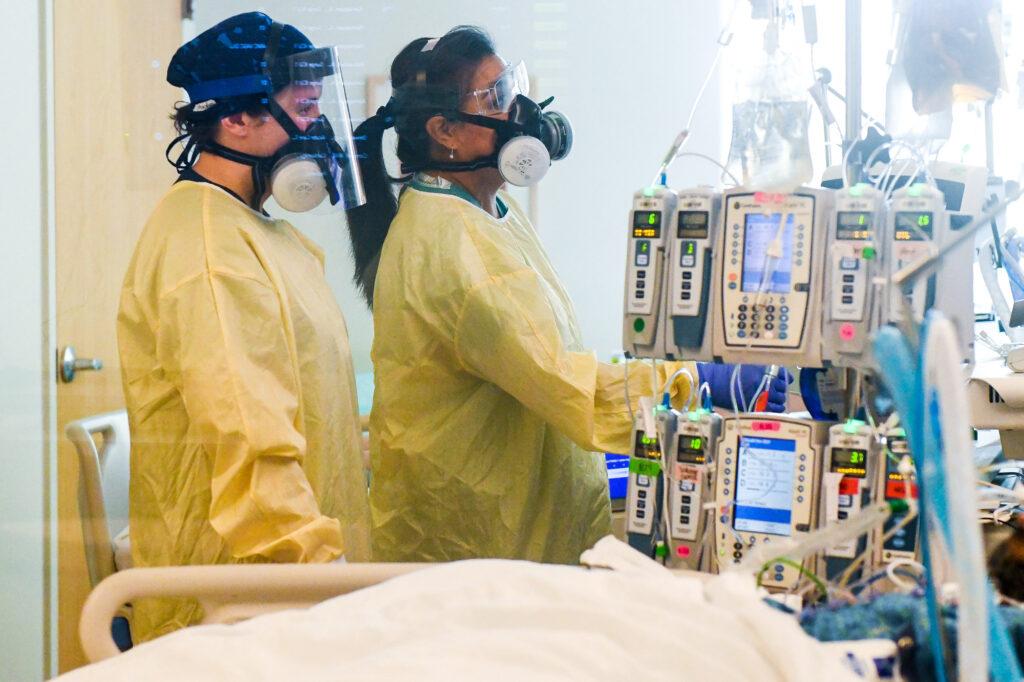
I meet people at various places through their hospital stay. Sometimes I meet them right in the emergency room. Sometimes I meet them after they've been in the ICU for several weeks or months. And a lot of my interactions are with family members because often people with COVID with really bad COVID are too sick to tell they're on breathing machines. They're sedated. So a lot of the work that I do is with family and letting them process what it's like to be afraid and to be angry. My approach is very similar to other families in the ICU is just to give them space, to process their grief and to normalize that this is scary and hard. And my goal often is just to give them space to voice those things on your heart that are hard to say.
Is there any story or stories that really stand out?
Early on in the pandemic? I remember a father and a son died on the same day were kind of back to that. Again, of families getting sick families who are not sick, trying to scramble and figure out what's going on. You know, maybe it's the one person who paid all the bills. And sometimes it's two parents that have kids at home. It's a ruthless disease. And we see people who don't believe in COVID who do believe in COVID when they're in the ICU. But it's, by that point, it's kind of too late to do anything about it, except pray with their families that they make it out of the hospital okay.
What do you hope the community will learn from this tragedy?
That we're all people trying to do our best? So I, I would just hope that after all of this, that we can come together because our common purpose is to try and keep our community healthy.
I assume that there are providers, doctors, nurses, respiratory therapists that also want to have somebody to talk to. Do you talk to them too?
You know, March 2020 is, was a really big turning point in how we moved about in our role and how we had to figure out how to support the people that we were working with before my job was maybe, like, 80% family and patient support and 20% staff support. And now it feels much closer to 50-50. The people I'm working with, the people who have stuck it out this long are really fried or they're brand new and seeing all this horror for the first time.
Do you have any final thoughts you'd like to share?
I think what I would want everybody to know is that you should get vaccinated. It is the thing that we can do for one another. And for ourselves, if you don't feel like you can get vaccinated to keep your immunocompromised neighbors safe, maybe you can do it so you can make sure you can be there for your kid's graduation.