One Colorado researcher is moving forward with a clinical trial to see whether the drug Leukine, normally used for bone marrow transplants and to treat some forms of cancer, reverses memory loss in people with Alzheimer's.
Huntington Potter, who directs the Alzheimer’s and Cognition Center at the CU Anschutz Medical Campus and the Alzheimer’s Disease Program at the Linda Crnic Institute for Down Syndrome, describes the latest research on Alzheimer's disease and the connection between Alzheimer's and both Down syndrome and rheumatoid arthritis. The disease affects about ten percent of people over 65 and about a third of people over 85. Nearly seven million Americans currently have Alzheimer's and that number is expected to almost double by 2050.
If you or someone you know wants to take part in the Leukine clinical trial, click here.
This interview has been edited for length and clarity.
During a TED Talk several years ago, the author of the best-selling novel, “Still Alice” spoke about Alzheimer's disease. She began by offering a sobering message to the audience.
Lisa Genova: “I think we all have this hopeful expectation of living into old age. Let's project out into the future to your future yous, and let's imagine that we're all 85. Now, everyone look at two people. One of you probably has Alzheimer's disease. All right, all right. And maybe you're thinking, "Well, it won't be me." Then okay, you are a caregiver. So in some way, this terrifying disease is likely to affect us all.”
That's neuroscientist and author, Lisa Genova, in 2017. “Still Alice” was eventually made into a movie.
We're going to talk today about what we know now about Alzheimer's as part of our series, Aging Matters on Colorado Matters. Huntington Potter directs the Alzheimer's and Cognition Center at the CU Anschutz Medical Campus. Potter says dementia and Alzheimer's are often used interchangeably, but they're each very different.
“Dementia is the big umbrella term for a cognitive problem in a person that relates to their memory, their executive function, their ability sometimes to just carry out their daily activities. And because it's a clinical description of a person's behavior, we now know that there are many mechanisms by which dementia can arise. And the reason that it often is confused or used interchangeably with Alzheimer's disease is because, in the elderly, the vast majority of the causes of dementia is Alzheimer's disease.
Now, if somebody has dementia at the age of 40, then the chances that it's Alzheimer's disease are much lower and you start looking for other problems. And the most common are, for instance, Lewy body dementia, which is related to Parkinson's, vascular dementia, which is related to atherosclerosis in the brain. And very often when a person dies and donates their brain to science, the pathologist may find that they have Alzheimer's, but they also have some vascular dementia. So mixed dementia is extremely common.”
| Whether you're aging yourself or caring for someone who is, what questions do you have? Email us at [email protected] or leave a voicemail at 303-871-9191 X 4480. |
Still, Potter says it's important to try to figure out if Alzheimer's disease is causing a patient's dementia or something else.
“Because the treatment of the patient and the future prediction of their disease course really depends on the kind of dementia that they have. To give you an example, if somebody has vascular dementia, then the treatment would be along the lines of lowering their blood pressure, lowering their cholesterol, and that would have a benefit in vascular dementia. But Alzheimer's disease is treated by these new drugs that are being developed for Alzheimer's disease, and they would have no benefit in somebody with vascular dementia.”
Potter points to a series of tests that can usually help give a doctor confidence that a person has Alzheimer's as opposed to another condition.
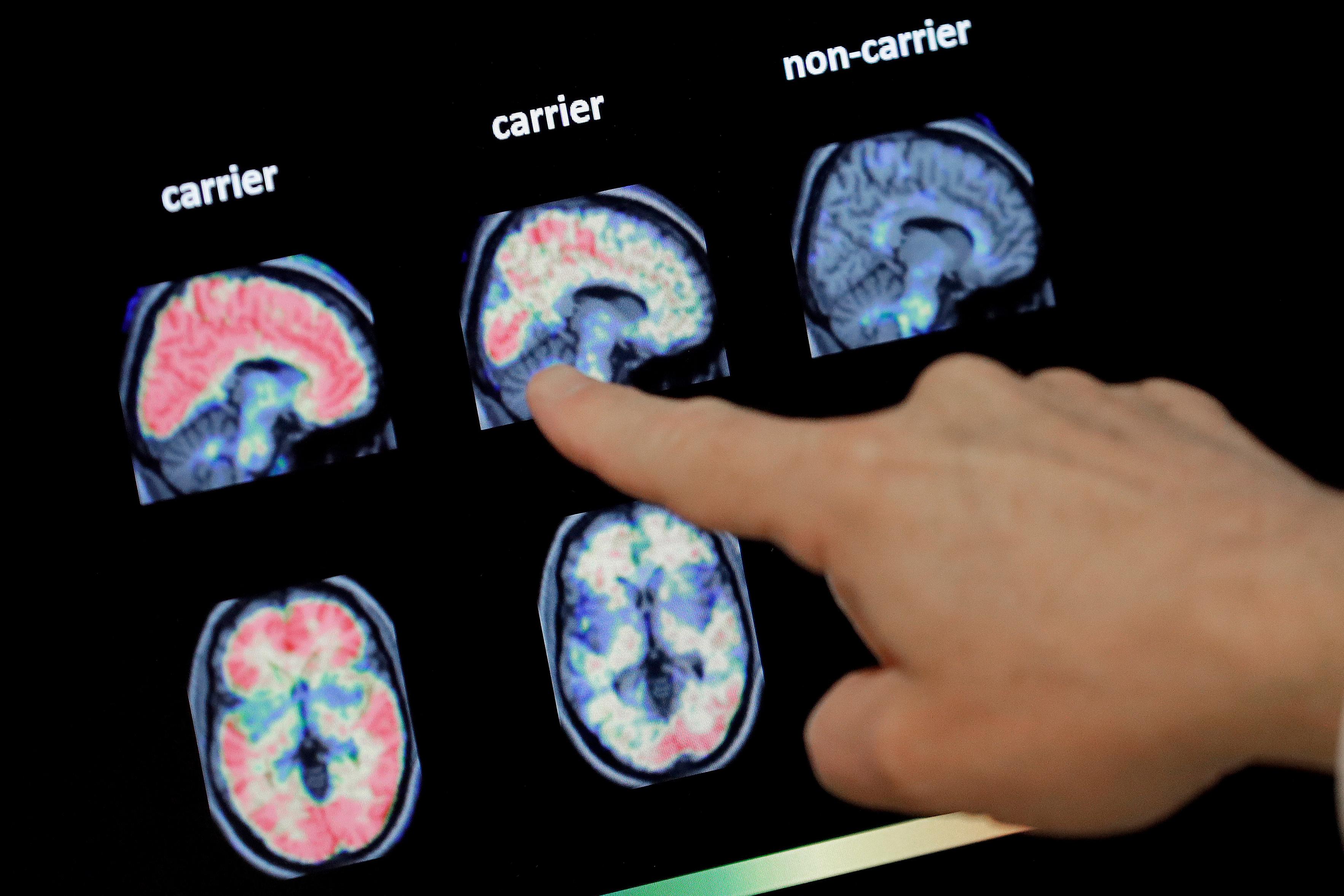
“This is a combination of neuropsychological tests, an interview of the family members, and a number of medical tests related to the blood. So there are proteins in the blood that can give an indication of Alzheimer's disease. There's proteins in the cerebral spinal fluid, so from a spinal tap, but you can also add confidence that the person has Alzheimer's disease. And then there are brain scans that are used to really add confidence that a person has Alzheimer's rather than something else. If the physician is a little unclear whether the person has frontotemporal dementia or Alzheimer's disease, then a brain scan can be definitive.”

Aside from tests, Potter says family members may also look out for clues.
“Anytime that somebody seems to have short-term memory problems, they may tell the same story multiple times, they may forget what they heard, somebody tell them five minutes earlier. It's the short-term memory deficits that is an indicator to the family. Of course, there are other features of people's lives, for instance, executive function related to can they handle their finances? And that is different for each person.”
The chances of getting Alzheimer's increases during the aging process. About 10 percent of people over 65 have some symptoms of Alzheimer's or dementia, and about 30 to 40 percent of people over 85. And here's another statistic; about two-thirds of patients are women, and many caregivers are also women. So Potter says it's important to understand why women are at a greater risk, and he makes a point that may be reassuring to some.
“There is a difference between normal age-associated cognitive decline that is what we would consider a normal feature of aging and Alzheimer's disease. And a behavioral neurologist, of which we have seven or eight in our memory disorders clinic, can tell the difference between normal cognitive decline due to age and Alzheimer's disease, which is a disease that is related to the formation of certain protein deposits in the brain, and the loss of neuronal function because of those. Age-associated cognitive decline, its mechanism is still under a lot of investigation.”
Potter says right now, there are only a few drugs currently on the market for Alzheimer's patients.
“In Alzheimer's disease, the primary defining neuropathological feature in the brain is a positive amyloid. Amyloid looks like millions of little Brillo pads in the brain made up of a protein called Abeta, and they result in the killing of neurons and the declining cognitive function. There are three drugs that have been FDA-approved for removing amyloid in the brain of a living Alzheimer's patient. The first one was called aducanumab, and then most recently there's lecanemab and donanumab. The ‘mab’ at the end means that they’re a monoclonal antibody, which is a protein that's been developed to attack amyloid. All of these drugs are very effective at removing amyloid from a living individual as measured by a PET scan that can see amyloid. The disappointment has come from the fact that instead of reversing Alzheimer's disease, they're merely able to slow the decline in the cognitive problems, and that's good. That's a major step forward, but it comes with caveats.
All of these drugs have side effects, similar side effects, and those side effects are bleeding into the brain and swelling of the brain that can be detected by an MRI brain scan and are sometimes clinically relevant. So that's a problem, and the sad thing is that the people with Alzheimer's disease who are most prone to these, what we call ARIAs for ‘Amyloid Related Imaging Abnormalities,’ are the people who have an APOE4 gene inherited from one of their parents.
And so most people who have Alzheimer's disease are APOE4 positive, and the problem is they are also most likely to develop an ARIA, an imaging abnormality of brain bleeding or swelling. So there's a caveat that the physician needs to take an APOE4 test for their patients and then talk to them about the risk of these side effects compared to the potential benefit. It's definitely not a no-brainer to go and take one of these drugs. They have benefit, but it's a slowing benefit, not a reversal benefit, and they have side effects.”
Dr. Potter's own research has focused on one particular drug, Leukine, and the research into Leukine for Alzheimer's has an interesting backstory.
“The study of Leukine or GM-CSF started more than a decade ago when we wanted to find out why people with rheumatoid arthritis tend not to get Alzheimer's disease. They're protected. And to make a long story short, we found this natural human protein that was increased in the blood of people with rheumatoid arthritis. And when it was injected in the brains or the tissue of mice, it reversed their Alzheimer's disease. Luckily, it was an FDA-approved drug already for other purposes, and we could do a clinical trial, which we published about a year and a half ago, and that's the first clinical trial that showed an actual improvement in the people who were injected with Leukine, the commercial version of GM-CSF. And there was a benefit in their blood biomarkers of brain damage.
That's great, but it was only a three-week trial. So the NIH then awarded us a grant to do a longer 24-week trial, and that is ongoing right now. Leukine has been FDA-approved for 30 years, and it essentially has no side effects of a serious nature that either we found in the Alzheimer patients or that have been found in the 30 years of its use for stimulating the bone marrow to make special white blood cells whose job it is to be little Pac-Men that go around the body and eat up things that aren't supposed to be there like amyloid in the brain.”
Other research institutions and companies are using different approaches to develop treatments that could at least partially reverse the cognitive problems in Alzheimer's disease.
“They're still in clinical trials. They've not been approved yet. The preliminary data look promising, but not so much for real reversal. Again, it's a slowing of the cognitive decline. Now, it's interesting that many trials and new drugs for Alzheimer's disease are being carried out by various people, including us here at the University of Colorado. But if somebody has already been put on one of these anti-amyloid drugs, then they're excluded from participation in the new trial of let's say Leukine or the others that are being tested because we don't want somebody who's already been treated to enter a trial and make it more confusing to interpret the results. So if you're going to go on Leucine, don't take aducanumab or leucanumab first.”
As for the hundreds, perhaps thousands of supplements advertised to help improve cognition, Potter says so far, no supplement has been shown in a proper clinical trial to have any benefit. And then there's the question of whether certain behaviors can reduce the risk of getting Alzheimer's or what's called MCI, “Mild Cognitive Impairment.” Potter says they can.
“Exercise and a good diet, general healthy behavior is able to slow things down and reduce the risk of conversion from mild cognitive impairment to Alzheimer's disease. And of course, in an elderly or even a middle-aged person, if you want to reduce your risk of developing MCI or Alzheimer's disease, then these behavioral changes have also been shown to be beneficial, both in the animals that are models of Alzheimer's and in people. Exercise, exercise, exercise is good for many things, including Alzheimer's disease. Of course, it's probably not a magic bullet that if you just exercise forever, you're going to avoid Alzheimer's.
And the other thing of course, is that there's a benefit to heart disease and stroke by also increasing your exercise regimen and eating more healthily and reducing your cholesterol and your blood pressure. So these kinds of things have a double benefit. As the Alzheimer's Association says, ‘What's good for your brain is good for your heart and vice versa.’”
| This story is a part of Aging Matters, a series from Colorado Matters about the Centennial State's aging population. Read more stories here. |
Dr. Potter also researches Down syndrome, and that's because there's a key connection between that condition and Alzheimer's.
“People with Down syndrome have two challenges with relation to their cognition. One is a natural feature of Down syndrome where they have some cognitive problems that they're born with. They will continue to have these for the rest of their life. Then as they get into their 30s, 40s and 50s, they also develop Alzheimer's disease, which adds on top of that cognitive problems, additional problems, but they are quite different. And the fact that people with Down syndrome all develop the Alzheimer pathology in the brain by the time they're 30 or 40, and most become demented by the time they're 50 or 60, but interestingly enough, not everyone with Down syndrome, has actually been a tremendous influence in the way we think about Alzheimer's disease in typical people.
And the reason is that people with Down syndrome have three copies of chromosome number 21, and the main Alzheimer gene is on chromosome 21 that makes those amyloid, and that means that they're going to develop amyloid faster and earlier than typical people. What that knowledge gave us was that the amyloid deposit is really an important starting place in all Alzheimer's disease, and that has informed the development of many of the diagnostics and the treatments for typical Alzheimer's disease that would also help people with Down syndrome.”
As for a timeline, Dr. Potter is hopeful.
“I started working on Alzheimer's disease about 20 years ago or more now, and every time somebody asked me that, I would say, ‘I think we will have a treatment in about five years,’ and that five-year horizon continues to retreat. But I think it is fair now that we know so much more about the disease and the potential treatments, and so many treatments are being tested in clinical trials that five years is a pretty reasonable prediction right now.”









