
Editor's Note: This story contains discussions of death, dying, physician-assisted suicide and medical aid in dying, which some readers may find uncomfortable.
A patient with terminal cancer approached Dr. Barbara Morris in 2019 for help ending his own life. The Colorado End of Life Options Act, which allowed for it, had passed with broad voter support just a few years prior. Dr. Morris worked for Centura Health, a Catholic system, which forbade her from offering such care. She filed suit — seeking judicial review — and was terminated just five days later. Her firing drew national headlines.
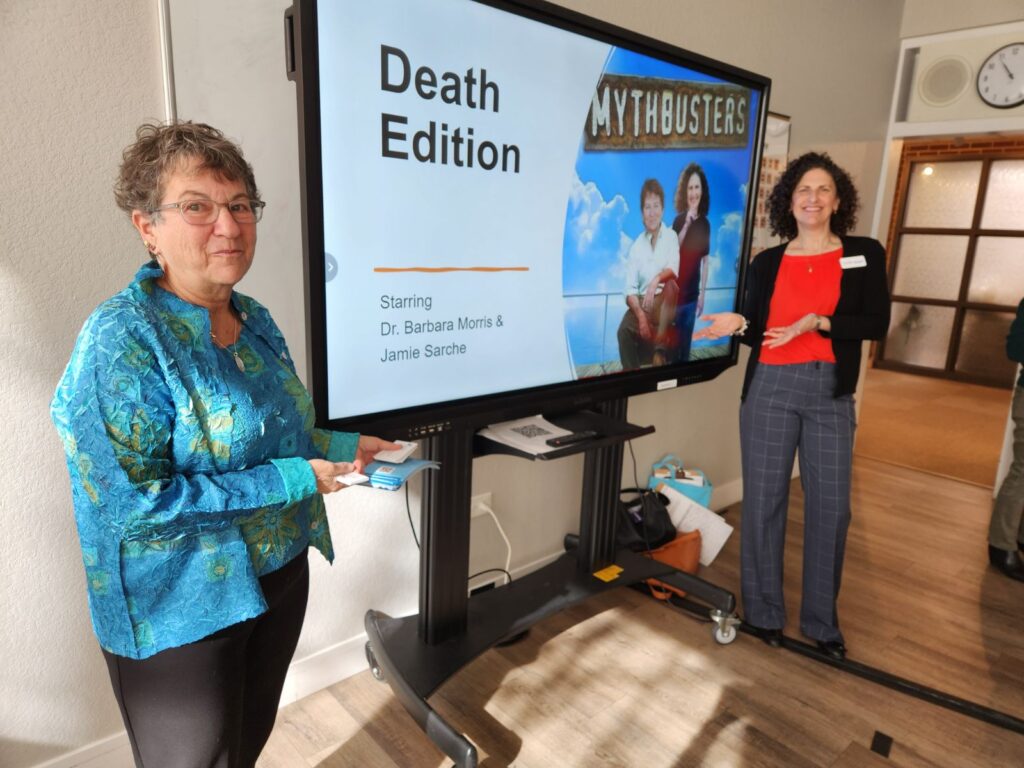
Five years later, the case is settled and the Denver geriatrician is on a path she never imagined for herself: advocate and educator. Dr. Morris now leads the fledgling non-profit End of Life Options Colorado. It educates patients, families, and clinicians on the state’s still-evolving aid-in-dying law, sometimes referred to as physician-assisted suicide.
Dr. Morris discussed her solemn work with Colorado Matters Senior Host Ryan Warner.
This interview has been edited for length and clarity.
Ryan Warner: In 2019, you sued your employer. For religious reasons, they barred you from raising with patients Colorado's then-new End of Life Options Act, and five days after you filed suit, you were fired. That case has since been settled. Remind us of the terminal patient at the heart of that case.
Dr. Barbara Morris: I was helping care for Neil Mahoney. His name has been public since this happened in 2019, and he wanted to stay with our office and his health system. He had a devastating terminal diagnosis and wanted to make use of medical aid in dying. At that time, there was a policy at Centura that prohibited any affiliated or employed physicians from participating in any aspect of aid in dying. We filed suit to ask the court to clarify whether that policy was legal, because the statute has language that we thought needed to be interpreted by the court. Five days after we filed, I was terminated from my position at Centura, which was very sad for me, for Neil, and for my 400 other patients.
Warner: Were you able to stay connected with Neil in his final days? And it was terminal cancer, right? Incurable.
Dr. Morris: Yeah, he had an incurable gastrointestinal cancer that was rapidly progressing. During that time — because I had been terminated— I did not have my own practice. I did not have any infrastructure, insurance, etc. so I couldn't continue as his physician, which was very devastating for all of us. However, I did stay in touch with Neil and his family through those months until he ended up dying. He was able to make use of medical aid in dying.
Warner: How often do you think about him?
Dr. Morris: I think about him a lot, actually. Neil taught me a lot, and I really admired his courage and his persistence. Not only was he interested in being able to make use of the law for himself, but he was determined that other folks would not face the same barriers.
Warner: I know you can't discuss the finer points of the settlement, but a multi-part question: Does any part of you feel vindicated? And two, I think it's still the law that a health system doesn't have to participate or allow their doctors to if it violates their views.
Dr. Morris: Yeah, so it is complicated. All I'm going to say about the settlement is that I am really glad that a very, very long and very stressful legal road is over. I think we've gained some clarity about this in the state, but there's probably still some issues that need to be further defined.
Warner: Say a little bit more about what the power is of an institution versus a doctor working for that institution. How do you understand it?
Dr. Morris: It's complicated. I always recommend now that clinicians make sure they know what they're signing when they sign their contracts. That might sound funny, but it's important. And the statute allows a health system to opt out of participating in aid in dying. The language is actually that they can opt out if the patient is planning to use the medication in their facility.
Warner: Do you think faith-based systems should be forced to offer care that's against their values?
Dr. Morris: I'm not usually speechless, but you got me, Ryan. I think that's, again, so complex. I think patients should have the ability to access our laws and care that they want and deserve in Colorado. And to the degree that faith-based systems have the right to uphold their religious beliefs, can sometimes come into conflict with what patients and physicians want.
Warner: You now lead a fledgling non-profit called End of Life Options Colorado, whose primary mission is education of individuals, families, and notably, medical providers. What are the most common gaps in knowledge when it comes to the End of Life Options Act for healthcare workers?
Dr. Morris: We have the whole spectrum. Two or three years ago, I had a patient's family where their primary care physician had just moved from another state, and when they inquired he said, "Well, it doesn't matter because it's illegal in Colorado." So that's one end of the spectrum. People who just…
Warner: Who don't even know that the law exists!
Dr. Morris: …and are giving patients— not out of any bad intent— but they're giving misinformation. On the other end of the spectrum, we have clinicians who are very supportive, who want to do the work and help their patients, but are either what I say, unable or unwilling. The “unable” is if they're in what I call a restricted setting. Their health system has said, "No." Or unwilling because they are well-informed, but for reasons of logistics, their practice style or their own personal beliefs, they're not going to participate. So between the, "I'm totally wrong," end of the spectrum and the well-informed spectrum, we've got a lot of clinicians in between.
Warner: What are some of the concerns or the obstacles for folks who would like to provide this kind of care but aren't currently doing so?
Dr. Morris: There are many. You're probably aware that both in primary and specialty care these days, physicians are under huge time pressure. So for some of them, it's just, "I'd really like to help with this. But it is time-consuming.” It's emotional for all of us when we work with these patients. And it can be somewhat stressful.
Warner: This is not a process you'd want to rush or fit in between appointments.
Dr. Morris: Correct. So that's a barrier. And for some of them, they have the basic knowledge, but just don't really feel like they're going to provide these services frequently enough, and don't feel up-to-date enough on the details.
Warner: Is continuing education the key?
Dr. Morris: Well, I'm very biased, so my answer is yes, absolutely. I like nothing better than doing a coaching or mentoring call with a colleague who's had a patient present who needs services and that colleague is willing. But we all need a lifeline, we need a friend. And those are the calls where I feel like I can make just-in-time impact in helping colleagues understand, have skills and have support.
Warner: It makes me think how good psychologists and psychiatrists have good psychologists and psychiatrists themselves to process the job with. It sounds like when you're talking about aid in dying, physicians who might engage in that kind of care also need that support.
Dr. Morris: Correct. I’ll give you two examples from this week. I talked with a physician in Leadville. She recently had a client who was requesting services. And we had a wonderful conversation. She was very open to more information, and I guess I'm proud because by the end of that call, she was willing to have her practice listed on our website where we list resources for patients.
Warner: To say to the public openly, "I do this."
Dr. Morris: Yes. Which in 2017, no one wanted to do. It was like a secret club. And I think we're past that time. The other quick example is I have a current patient, and she had developed a very lovely relationship with her nurse practitioner who does home visits. She kept saying to me, "Please have her come." We need a consultant as the second to the attending clinician.
Warner: Right. You need two clinicians.
Dr. Morris: So here was this nurse practitioner and I called her and I said, “Are you aware of the law, and are you aware that you can act as the consultant? And here's what it would take." And she said yes. I sent her a lot of information. She saw the patient. She did the consultant letter that I required. It was a beautiful thing.
Warner: “A beautiful thing” because I gather if you have a terminal illness and you have grown comfortable with your providers, the last thing you want is to have to introduce someone new.
Dr. Morris: Correct. And you certainly don't want to have to introduce two new people.
Warner: The law has been updated since voters passed it overwhelmingly, and that expands who can be signing off on this stuff.
Dr. Morris: That's correct. So Governor Jared Polis signed the amended law over the summer. The two big changes are that we decreased the waiting period from 14 days to seven, and we added advanced practice nurses who have prescriptive authority. They can act as either the attending clinician or the consulting clinician.
Warner: So the changes then pick up the pace. Why is that important? Because I can imagine someone listening saying, "Well, let's not go too fast here."
Dr. Morris: Right. Well, first of all, sometimes patients have a rapidly-progressive illness with a tremendous amount of suffering, and waiting 14 days could be really unbearable for them.
Warner: Especially because you have to self-administer the drug.
Dr. Morris: That's correct. And sometimes patients don't even find out that it's a choice until they're really far along in their illness. So they then are like, "I want to do this now." And it's because of suffering. That's what patients are trying to deal with.
Warner: Any other changes you wish could have happened that did not?
Dr. Morris: Yeah, there were two that I'd like to see us work on in the future. One is residency. People may remember that our statute requires Colorado residency to proceed, which is a little unusual in terms of medical care. We don't require that for other things, except there might be some issues with reproductive rights now. But otherwise, in medical care we don't require residency.
Warner: But there's a fear that Colorado somehow becomes the state you travel to to die.
Dr. Morris: Right. There is a fear of that. I'm obviously, again, biased about this. I’m not too worried about that as an issue really. Because remember, people are in a terrible time in their lives if they face a terrible illness with a bad prognosis and no available treatments. People are not going to move here at a whim. It's hard. So I think getting rid of the residency doesn't pose a lot of threat for Colorado at all.
Warner: Some disability rights advocates feared that laws like this cheapen life, especially for people with disabilities who might be viewed as easier to dispatch with than to care for. Have you seen that or other perverse outcomes?
Dr. Morris: I've never seen that. I've never seen a perverse outcome. I can only speak for my own experience and my colleagues'. One of the things about our statute, and the statutes in the other jurisdictions, is there are quite a few guardrails. The colleagues I work with and the clinicians I mentor and coach take this very, very seriously. And we all want to work with high integrity and within those guardrails and within ethical boundaries.
Warner: And if you don't, who's there to hold you accountable?
Dr. Morris: That is a really interesting question. I think our community holds us accountable, our colleagues hold us accountable, and ultimately the state holds us accountable, although it may not be in as direct a way as you're thinking.
Warner: A few years ago, some case studies emerged of people with anorexia who used aid-in-dying medication with help from a Colorado doctor. What did you make of that? What do you make of that?
Dr. Morris: I'm not going to comment on the specific cases, of course. The topic is one that is being debated actively all over the United States and in Colorado. And I think we have to accept that there's disagreement among very well-versed clinicians, very well-intentioned physicians about what is the meaning of a terminal diagnosis and a prognosis of less than six months. And for me, I put it in that framework.
Warner: I might add for context that anorexia as a mental health disorder, I think is one of the deadliest there is.
Dr. Morris: That is correct.
Warner: I remember, when the law was being debated, conversations about the comfort merely of having the medication, and perhaps never using it. That a patient felt empowered perhaps by the having of it. Have you seen that borne out?
Dr. Morris: I haven't seen it in my own personal practice, but we know the data all over the country and in Colorado parallels, which is about, believe it or not, 30% of patients will go through our whole process, which is not simple. People want to be heard. They want us to recognize their suffering. They want to know that if their suffering becomes just intolerable, that they have a choice. It's about choice and respect for these patients.
Warner: Indeed, you've educated communities around this state as to the law. You've been to Durango, Grand Junction, Salida. I understand you even walk providers through some of their first few cases. What's that like?
Dr. Morris: We have met amazing people on these trips. We try to do both public education, and then if possible, I like to meet with a group of clinicians to dig into the more medical stuff. And as a result of those, I've often gotten a call from a clinician saying, "Hey, I heard about your presentation. I saw your presentation. Can you help me?"
Warner: I wonder if providers ask you what they should charge.
Dr. Morris: Yes. The reason clinicians are having this conversation is that there's a federal law from the 1990s that prohibited any federal dollars going towards what was defined as assisted suicide. That's complicated because our law says that aid in dying is not assisted suicide or euthanasia, but the legal world has debated that. And so Medicare, and in most states, Medicaid — because of fears of being sanctioned or losing money — will not pay for services related to aid in dying, nor will they pay for medications.
Warner: Then you face the question of, if it becomes private pay, do you have a system in which wealthier individuals are at an advantage somehow or have more access?
Dr. Morris: Absolutely. If we look at the demographics in Colorado, we know this is mostly a white, middle and upper class population. I don't think it's only because of money, though. I think it's because of education and access. I think it's because of communication and cultural awareness that we have some of that, but part of it is money for sure. And the price of medications has skyrocketed as many things have. And as an organization, we are working to make sure that patients have an ability to get some assistance, particularly with the medications if need be.
Warner: Is this making it into medical schools?
Dr. Morris: I can't answer that completely. I think in a broad way, it's getting into medical schools, but as with many topics, it's probably brief and not with a lot of clinical experience. So over time, one of the initiatives we have to talk about is getting more in-depth information into medical schools.
Warner: How often are you saying, "You don't qualify" [under Colorado’s medical aid-in-dying law]?
Dr. Morris: In the past year, I've had two clients, and this is one of the hardest things I actually have to do, who I said, "I'm sorry, but you're not appropriate." For whatever reason. And it's really hard. People are suffering. They have chronic illness or they have other illnesses.
Warner: Chronic, but maybe not terminal— and yet may feel terminal.
Dr. Morris: It may feel terminal. But we're in the United States. Our laws have been written in a certain way. And I say the United States, because sometimes we tell people they can explore other options in other countries. And sometimes that helps, sometimes it doesn't. I'll tell you what my patients and their loved ones do understand is I say, "Look, this law is really important for Coloradans, and it's really important that we follow it properly and have high integrity because we don't ever want to risk an issue with the law, and we want Coloradans in the future to be able to access this care." And you know what? They say, "I understand."
Warner: It makes me think you feel like you're under the microscope still though?
Dr. Morris: Oh, yeah.
Warner: People are watching. Are they waiting for you to make a mistake?
Dr. Morris: I don't think they're waiting. I'm watching myself.
Warner: Reflect on the last five years for us, since what you call your “forced sabbatical.” Did you ever think you'd be where you are today?
Dr. Morris: No. When this whole thing started, Ryan, you'll recall from our conversation five years ago, I was a practicing geriatrician. I thought that aid in dying should be a tool in my toolbox. I was not involved with the original legislation. Supportive, but not involved.
Warner: You were not an advocate.
Dr. Morris: No. I was just like, "Great. This is something I think my patients should have access to." Well, if you fast-forward, I got catapulted by what happened into doing work in the state when I realized how much need there was for education and access and services. And so now I find myself as president of this organization, and I'm proud to be doing that work. It is not where I expected to be. When I wrote to Neil [Mahoney]’s brothers to tell them we had founded End of Life Options Colorado, one of his brothers said, "Well, Neil would be proud. This is the work you were meant to be doing."
Warner: Do you think about your own access to this care if you should need it?
Dr. Morris: Oh, of course I do. I've been doing geriatrics and end-of-life care for decades. So thinking about my own potential illness or mortality is not a new question, but aid in dying is a specific way to handle end-of-life. And I'll just tell you this, every patient I work with, especially when I have the honor of attending at the time of ingestion and medication, I am just so amazed by the courage, the resolve of these patients, that this is what they need to do and want to do. And I sometimes wonder whether I would be able to do that.








